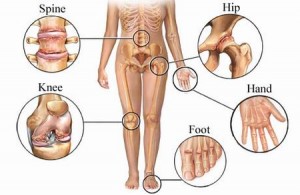
Arthritis is a general term, meaning inflammation of joints. Osteoarthritis is the most common form of arthritis and is of degenerative type. It may occur in any joint of the body but it is more frequently observed in joints receiving the highest loading. These are the knee, hip and spinal joints.
Articular cartilage is the tissue covering the end of the bone in every joint. The normal cartilage is smooth and its function limits bone friction by absorbing vibrations. So, it serves as an absorbing sponge receiving pressure, changing shape and reducing forces exerted behind it.
Osteoarthritis induces degeneration of the articular cartilage, which gradually loses its elasticity and absorbsiveness. The surface of the cartilage in time becomes more rough and brittle and in many cases fragmentation of small particles occurs inside the joint.
As vibrations are not absorbed, forces are transmitted to tendons and ligaments of the joints, which in most patients do not have the necessary muscle strength support to receive additional loading and, as a result, cause inflammation and pain.
Approximately twenty million Americans suffer from osteoarthritis. The disorder occurs over the age of 60 years but also a number of younger people, between 20 and 30 years of age, present with symptoms of osteoarthritis.
AETIOLOGY OF OSTEOARTHRITIS
- Heredity. Some people are born with anatomical abnormality of certain joints (knee, hip) or of the spine (scoliosis), which as time passes, turns into osteoarthritis more easily. Some others are born with a genetic predisposition to develop degeneration of articular cartilages.
- Obesity. It is an additional aggravating factor, causing osteoarthritis in the joints that receive high loading, such as knee, hip and facet joints of the lumbar spine. The loss of weight reduces pain and slows down progression of the disease.
- Injury. Injury of a joint, a bone or the spine, predisposes for osteoarthritis, Athletes exerting repeated forces on their joints that in time become traumatic, develop osteoarthritis from a young age.
- Pain and stiffness with movement
- Pain due to excessive overuse of the joint and after periods of inertia
- Oedema of the joints and hydrathrosis (hydrathron)
- Joint deformity
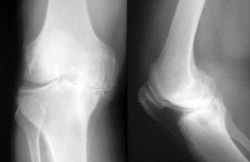
- History
- Physical examination
- Radiological examinations
TREATMENT
The treatment of osteoarthritis includes:
- Weight loss
- Μuscle strengthening
- Kinesiotherapy
- Physiotherapy
- Cold patches applied on painful joints (particularly after exercising)
- Drugs
- Intra-articular drug injection
- Surgery
Loss of weight reduces the loading exerted upon painful osteoarthritic joints and, consequently, limits pain. Strengthening mainly of the anterior thigh muscles leads to better absorption of knee joint vibrations.
Preferable are exercises which do not strain the joints, such as swimming and walking on soft ground wearing sport shoes. On the contrary, exercises that should be avoided are running (particularly on hard non-absorbsive surfaces) and intense aerobics training.
After any kind of physical exercise, ice therapy of the painful joints is imperative. The ice is applied upon the joint for 20 minutes. Between the ice and skin a thin wet towel is placed to protect the skin from a cold burn. Ice therapy should be repeated several times a day, particularly when the joints are quite loaded during the day.
DRUGS
- Paracetamol
- Non steroid anti-inflammatory drugs
- Duloxetine
- Opioids (tramadol, tapendadol, oxycodone etc.)
In the beginning, the pain is treated with paracetamol, which does not cause side-effects in the gastrointestinal and cardiovascular system. However, the long term and daily administration of paracetamol may cause drug-induced nephropathy that is reversible though, with the discontinuation of the drug. The daily dose of paracetamol should not exceed 3 grams due to the risk of acute hepatic failure.
Non steroid anti-inflammatory drugs should be administered for a short period of time and only if there is no contraindication. Definite contraindications are the history of cardiopathy, arterial hypertension and sensitivity of the gastrointestinal system to irritants which could cause haemorrhage.
Duloxetine (Cymbalta), a drug from the category of antidepressants, has recently been approved by the American Food and Drug Association (FDA) for the treatment of osteoarthritis. Duloxetine is a serotonin, norepinephrine reuptake inhibitor (SNRI) antidepressant, which has also been approved for the treatment of painful diabetic polyneuropathy and fibromyalgia. Some initial studies demonstrate its efficacy in impoving osteoarthritic pain and functional ability, considering that part of the osteoarthritic pain is of neuropathic pain.
Hyaluronic acid is a biological substance normally located in joints. It is a material which “feeds” the articular cartilage and is also a macroscopically viscous substance acting as lubricant in the knee and hip joint. It has been extensively used in early knee osteoarthritis and recently started being applied in the hip joints in cases of early degenerative lesions. However, it does not cure osteoarthritis; it rather improves pain, reduces stiffness and in many cases delays the performance of a surgical joint reconstruction.
Intra-articular injection of corticosteroids is applied when the pain is very strong and does not subside with the previous measures. Usually the result is impressive, but the duration of the result is not predictable and varies from case to case. It can be applied three times a year. Hip intra-articular injection is conducted under fluoroscopy by an expert physician specialised in the specific technique. Knee intra-articular injection can be done in the physician’s office without fluoroscopic guidance.
When the patient is not adequately relieved with the previous therapeutic measures and surgery is contraindicated, then opioids are administered, such as tramadol or tapendadol, oxycodone etc. which are tolerated by the patient, in relation with any possible concomitant disorders from the cardiovascular and gastrointestinal system.
None of the drugs inhibits or delays the gradual degeneration of articular cartilages.
ALTERNATIVE TREATMENT
Some studies demonstrate that supplements glycosamine and chondroitin reduce pain and improve the stiffness of painful osteoarthritic joints, particularly the knee. There is no evidence that glycosamine helps in the regeneration of the articular cartilage.
Conventional acupuncture and electric acupuncture may contribute to reducing pain.
INTERVENTIONAL PAIN TREATMENT
There are recent studies and case reports on osteoarthritic pain, where intra-articular pulsed radiofrequency was found to give significant pain reduction.
Larger and more reliable studies are needed to establish the efficacy of the previous therapeutic technique in the treatment of osteoarthritic pain.
If the conservative treatment fails to relieve the patient from pain or the patient’s ability for simple daily physical activities is limited, surgical treatment is indicated.
There are various types of surgical procedures:
- Arthroscopic joint debridement from free particles of the degenerated articular cartilage and cartilage trephination.
- Total knee or hip arthroplasty. Arthroplasties can be performed in other joints as well, such as shoulder and fingers/ toes.
Consult your physician about the treatment you should follow.