GENERAL
 Herpes zoster is caused by the Varicella Zoster Virus (VZV). When a patient has been cured from varicella, the VZV still remains in his/her body. This usually does not create any problems to the patient. However, years later, the virus may flare up and provoke herpes zoster.
Herpes zoster is caused by the Varicella Zoster Virus (VZV). When a patient has been cured from varicella, the VZV still remains in his/her body. This usually does not create any problems to the patient. However, years later, the virus may flare up and provoke herpes zoster.
Herpes zoster is manifested with a blistering erythematous rash, severe pain and pruritus. Approximately 25% of healthy adults will present herpes zoster, mainly over the age of 40. For individuals who have already been sick in the past with varicella, herpes zoster is not contagious. However, for those who have not been sick with varicella, contact with a patient who has herpes zoster may transmit varicella to them. The fluid content of the skin-rash blisters in herpes zoster contains the virus and transmits it to other individuals. Grandparents suffering from herpes zoster are very likely to transmit varicella to their little grandchild, whereas the opposite is impossible.
The incidence of herpes zoster increases with age. The disease is 10 times more likely to occur in adults over 60 years old than to children under the age of 10.
Individuals whose immune system is very weak, due to a disease or due to specific drugs that suppress the body defensive system (immunosupressants, chemotherapy, corticosteroids ) are in high risk for developing herpes zoster.
PATHOPHYSIOLOGY
The pain in herpes zoster is caused by the inflammation of sensory nerve terminals. The pathophysiology is not fully known yet. Two factors seem to play a major role: sensitization and interruption of sensory nerve fibers.
Peripheral (distal) sensitization occurs because some inflammatory agents -such as substance P, histamine and cytokines- reduce the stimulation threshold of nociceptors. Central (proximal) sensitization comes as a result of the increasing response of the spinal occipital horns to the continuous stimulation of the nociceptive C nerve fibers. The interruption of sensory nerve fibers may be due to the virus within the cell and the inflammatory reaction that follows. The oedema accompanying the inflammation may exert pressure on the sensory ganglion located in the intervertebral foramen and, thus, may lead to ischaemia and damage the nerve tissue. In addition, the activation of Schwann cells may be playing a further role in the whole process.
DIAGNOSIS
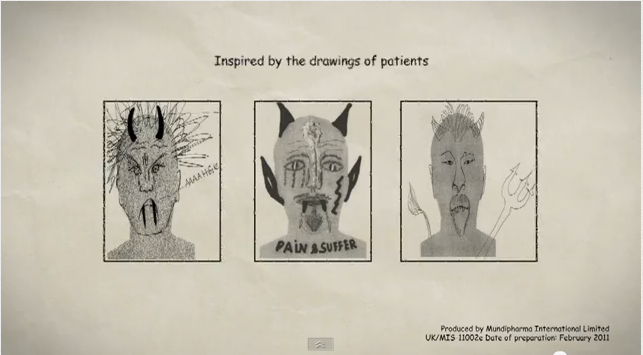
Patients with herpes zoster present unilateral symptoms in the dermatome corresponding to the spinal ganglion that has been affected. Besides pain, there are also paraesthesia, dysaesthesia and pruritus. Other symptoms that may be reported are fatigue, fever and headache. These last symptoms usually occur only a few days before the appearance of the rash. The pain is described as burning with concomitant numbness and pruritus. Patients with postherpetic neuralgia describe pain as “an acute, burning, pressing pain”, persisting steadily in the dermatome where the rash was located. There is usually allodynia and hyperalgesia. For these patients, even skin contact with clothes may be very unpleasant and cause them discomfort.
TREATMENT
The targets of herpes zoster therapy are the following:
1. Reducing pain intensity and duration
2. Restoring any probable skin defect and preventing secondary infections
3. Limitation or prevention of postherpetic neuralgia
The target of the treatment for postherpetic neuralgia is pain relief and improvement of the patient’s quality of life.
CONSERVATIVE TREATMENT
Α. Pharmacotherapy of herpes zoster
Antiviral drugs. Antivirals, such as acyclovir, famcyclovir and valacyclovir, should be taken the soonest possible after the onset of clinical signs. A review study has demonstrated that the initiation of antiviral treatment within 72 hours from the appearance of the first blisters, accelerates their healing by 1-2 days. However, it is doubtful whether the antiviral therapy can prevent postherpetic neuralgia.
Corticosteroids. A large randomized study compared acyclovir monotherapy with the combination therapy of acyclovir and prednisolone (corticosteroid) and found out that there was higher pain relief within the 2 first weeks in the combination group (antiviral + corticosteroid). However, the combination treatment had no effect in the healing of blisters.
Analgesics. Clinical experience has shown that non-steroid anti-inflammatory drugs and paracetamole reduce acute pain. Should pain persist, mild opioids can also be used (e.g.codein and tramadole).
Local anaesthetics. Both clinical experience and one randomized controlled study have demonstrated that the local application of lidocain is effective in reducing pain without any serious side-effects.
Concomitant analgesics. A small placebo-controlled study has shown that amitryptilin (25mg daily for 90 days) during the acute phase of herpes zoster reduced the risk for postherpetic neuralgia by 50%. Another study has demonstrated that gabapentin reduces pain in acute herpes zoster.
Β. Pharmacotherapy of postherpetic neuralgia
The treatment is similar to those for other neuropathic pain syndromes. The only drugs approved by the American Food and Drug Association (FDA) for postherpetic neuralgia are pregabalin (Lyrica) and gabapentin (Neurontin).
Tricyclic antidepressants. The most commonly used tricyclic antidepressant for postherpetic neuralgia is amitryptilin (Saroten). Various randomized controlled studies (RCT) have shown that the number of patients needed to treat for achieving at least 50% pain relief was 2,6 (NNT of 2,6).
Antiepileptic drugs. The respective number NNT for achieving at least 50% pain relief for gabapentin (Neurontin) was 4,4. The doses of this drug in the studies carried out ranged from 1800 to 2400mg. Pregabaline (Lyrica) has an action mechanism similar to gabapentin but with a better profile and with doses ranging from 150 to 600mg.
Tramadol. Studies have demonstrated that tramadole, in a dose between 200 and 300 mg daily, provides significant pain relief and improvement of the patient’s quality of life.
Opioids. A large randomized controlled study has shown that opioids are effective in the treatment of resistant neuropathic pain (NNT for the treatment of pain in postherpetic neuralgia was 2,7).
A randomized controlled study (RCT) has shown that the capsaicin dermal patch 8% has a highly effective analgesic effect, only with one single application to the painful skin area. The application is conducted only by physicians who have been trained in the performance of this therapy and are specially accredited by the company producing the drug (Qutenza).
 The above drugs can be administered also in combination, according to the judgment of the therapist physician and the probable limitations depending on the case history of each patient.
The above drugs can be administered also in combination, according to the judgment of the therapist physician and the probable limitations depending on the case history of each patient.
Stellate Ganglion Block
NTERVENTIONAL TREATMENT
1. Epidural injection. It has been shown that the intensity of pain is being limited in the acute phase of herpes zoster when a solution of corticosteroid and local anaesthetic is injected epidurally at the spinal level corresponding to the painful dermatomes. According to evidence-based medicine, epidural infusion is positively recommended .
As for pain relief in postherpetic neuralgia, the positive results for epidural infusion are based on individual case studies and observation studies. Its efficacy is not evidence-based, so the recommendation is neutral.
2. Sympathetic block. Its efficacy is not evidence-based either for the acute phase or the postherpetic neuralgia.
3. Neuromodulation techniques. Application of peripheral nerve stimulation or spinal cord stimulation with the use of an implanted generator and electrodes. These are performed in cases of resistant postherpetic neuralgia, when all pharmaceutical and less invasive treatments have been tried but the pain still continues to persist. There are no randomized controlled studies carried out yet, with regard to neuromodulation techniques.
MEDICAL INFORMATION SOURCES
1. PAIN PRACTICE JOURNAL
2. BONICA”S MANAGEMENT OF PAIN
3. PAIN PHYSICIAN JOURNAL
4. INTERVENTIONAL PAIN MANAGEMENT BOOK
5. NEUROMODULATION JOURNAL